NRS493 PICOT Question Sample Student Approach
Diabetes is a global health issue that negatively affects patient health outcomes. Nurses evaluate their environments to determine problems and plan effective evidence-based interventions. This paper develops a PICOT question for diabetes management and determines interaction with nursing practice, nursing intervention, healthcare agency, and patient care.
The PICOT question is: In Hispanic diabetic women between ages 45-60, does diabetes education using diabetes education checklist (standardized terminology) compared to traditional diabetes education improve diabetic patient follow-up visits in six months?
Patient education is an effective evidence-based solution in improving patient outcomes. A structured patient education program will ensure all patients receive uniform, comprehensive education on self-management to increase their self-efficacy. According to Chatterjee et al. (2018), patients who received structured education reported better self-efficacy and better readings of glycemic control parameters such as fasting blood sugar and HbA1c tests and post-prandial glucose tests.
Hence, patient involvement in diabetes management through extensive education is the cornerstone of effective glycemic control and the stability of other diabetic tests. Patients take time to learn, implement and master proficiency in performing learned tasks (Lee et al., 2019). Allowing patients some time to form the habit of portraying the required behavior ensures the data collected adequately reflect on patient education’s effectiveness. Six months is enough period to ensure the impact of structured patient education is evident hence
Diabetes is a clinical problem that is significant to patient outcomes. Diabetes complicates the management of other conditions and increases the risk of infections, hypertension, and peripheral vascular diseases. Most inpatient and outpatient management interventions entail patient-directed interventions, hence the need for patient education. Patient education is an effective evidence-based intervention, as seen in many studies (Nassar et al., 2019; Chatterjee et al., 208; Seeman, 2019; Zheng et al., 2019).
According to Nassar et al. (2019), patient education enhances patients’ initiative and responsibility. Educated patients also adhere to medications and treatment regimens more than uneducated ones. According to Zheng et al. (2019), patient education improves patient adherence to prevention and management interventions such as diabetic foot examinations, eye examinations, and HbA1c tests. Educating the patients helps prevent the negative psychological symptoms such as depression and anxiety associated with newly diagnosed diabetes. Patient education is thus an ineffective nursing intervention in controlling diabetes.
The target population for the PICOT question is Hispanic diabetic women. Hispanic patients are more exposed to diabetes and diabetes complications because of genetic predisposition. Adults between the ages of 45-60 often have more educational needs. Many older adults lack formal education hence the need for comprehensive, structured, face-to-face patent education. The education delivered should not miss any detail, and traditional methods have no specific pattern increasing the possibility of missing out on vital details (Chatterjee et al., 2018).
Patient education for diabetes helps achieve the overall healthcare agency goals; improves patient outcomes. Patient education is an important nursing intervention in improving patient outcomes for many healthcare conditions. Increased knowledge translates into responsible care and collaborative interventions (Seeman, 2019). Patient education also enhances patient collaboration in care provision, promoting better healthcare outcomes.
Effective patient education depends on existing organizational policy guidelines. A structured patient education program will ensure uniform and effective patient education for effective diabetes management. Nurses should focus on delivering comprehensive and quality education to ensure better patient responsibility among the selected population and collaborative interventions hence better patient outcomes and improved nursing practice. In addition, face-to-face education is an effective intervention for this age-specific group.
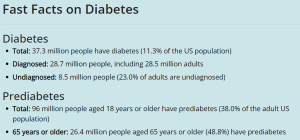
CDC Data on Diabetes
References for NRS493 PICOT Question Sample Student Approach
- Chatterjee, S., Davies, M. J., Heller, S., Speight, J., Snoek, F. J., & Khunti, K. (2018). Diabetes structured self-management education programs: a narrative review and current innovations. The Lancet Diabetes & Endocrinology, 6(2), 130-142. https://doi.org/10.1016/S2213-8587(17)30239-5
- Lee, S. K., Shin, D. H., Kim, Y. H., & Lee, K. S. (2019). Effect of diabetes education through pattern management on self-care and self-efficacy in patients with type 2 diabetes. International journal of environmental research and public health, 16(18), 3323. https://doi.org/10.3390/ijerph16183323
- Nassar, C. M., Montero, A., & Magee, M. F. (2019). Inpatient diabetes education in the real world: an overview of guidelines and delivery models. Current diabetes reports, 19(10), 1-8. https://doi.org/10.1007/s11892-019-1222-6
- Seeman, K. (2019). The importance of quality perioperative patient education. Journal of Consumer Health on the Internet, 23(1), 94-101. https://doi.org/10.1080/15398285.2019.1574525
- Zheng, F., Liu, S., Liu, Y., & Deng, L. (2019). Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: a randomized controlled trial. Journal of diabetes research, 2019. https://doi.org/10.1155/2019/1073131
Example Journal
Project Capstone and Practicum Reflective Journal
This week has been a tough one yet fun. I had a lot of activities regarding my project. First, I had to appraise articles and then come up with objectives for my projects. Besides, I found some time to hold a discussion with my mentor about ethical considerations in healthcare. I used my good communication skills and critical thinking while holding the discussion.
Understanding ethics is a vital requirement that every healthcare must do. Because ethics define our daily interactions with patients and defines the reasoning behind every activity starting from diagnosis and extending to management and follow-up. Essentially without ethics healthcare organizations would be in a total mess.
To begin with, ethics defines the standard code of conduct and moral codes. Four main principles of ethics are considered in healthcare; autonomy, justice, beneficence, and non-maleficence (Rao, 2020). These principles are both applicable to patients with no superiority whatsoever. In autonomy, every patient has a right to make decisions regarding what should be done with their bodies. Healthcare providers can only offer guidance but can not alter a decision made regardless of its consequences.
While beneficence requires healthcare providers to offer quality care, non-maleficence requires doing no harm. In addition, justice requires fairness while making decisions (Rao, 2020). Maintaining and working according to ethics brings harmony even when dealing with a culturally diverse population. This is because different cultures have basic requirements that must be fulfilled and may affect the health and health-seeking behavior of some individuals.
Therefore, there is a need to equip all healthcare workers with knowledge of ethics. In addition, all rights of patients must be acknowledged and respected. Because rights are universal and define our relationship with patients. Finally, failure to observe ethics and patients` rights is a weakness of most healthcare workers which could deteriorate relationships and negatively impact health.
References
- Rao, P. R. (2020). Ethical considerations for healthcare organizations. Seminars in Speech and Language, 41(3), 266–278. https://doi.org/10.1055/s-0040-1710323
Also Read: NRS493 Literature Evaluation Table Paper
