FNP NR511 Week 3 Case Study Part 2 Example
FNP NR511 Week 3 Case Study Part 2 Example
National Patient Safety Goal 1
Patient with bilateral eye discomfort
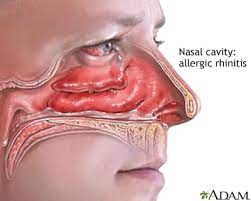
My primary diagnosis is Allergic Rhinitis (ICD 10 code H10.13). The patient presents with bilateral itching of the eyes, redness, discomfort, and tearing of the eyes. These are definitive symptoms of allergic rhinitis. Physical examination of the eyes elicits a slight sensitivity to light. This is also a common finding in allergic conjunctivitis. FNP NR511 Week 3 Case Study Part 2 Example
Medication.
Pharmacological treatment involves the use of OTC antihistamines, vasoconstrictor drops, mast cell stabilizers, NSAIDS and corticosteroids.
- Olopatadine ophthalmic solution 0.2%. for allergic conjunctivitis, administer 1gtt in the affected eye once every 12 hours. Continue administering the drug even in the absence of symptoms as long as there is exposure to the agents that can cause allergic conjunctivitis. FNP NR511 Week 3 Case Study Part 2 Example
 Olopatadine is an antihistamine-mast cell stabilizing agent. It is considered as one of the first line drugs for allergic conjunctivitis. They are effective in controlling inflammation and providing acute symptomatic relief. Because it is dual acting, it exhibits a high degree of effectiveness.
Olopatadine is an antihistamine-mast cell stabilizing agent. It is considered as one of the first line drugs for allergic conjunctivitis. They are effective in controlling inflammation and providing acute symptomatic relief. Because it is dual acting, it exhibits a high degree of effectiveness.
Olopatadine doesn’t penetrate the blood brain barrier and is therefore unlikely to induce the CNS effects associated with other antihistamine agents. This drug can also be used regularly without long-term safety concerns. It also has no drug interactions
- Flonase (fluticasone propionate) Nasal spray 16g. spray once in each nostril twice daily or as needed.
The patient should resume taking his fluticasone medication because the clinical findings reveal that he has symptoms that might be related allergic rhinitis. He also has a past medical history of seasonal allergic rhinitis and therefore this medication could be beneficial to him. Fluticasone is a corticosteroid. Corticosteroids have anti-inflammatory properties and modify the body’s immune response. They have been shown to be effective in alleviating signs and symptoms of allergic rhinitis and allergic conjunctivitis. The patient presents with runny nose with occasional nasal congestion, pale and boggy nasal turbinates and watery eyes. This nasal spray could relieve some of these symptoms. FNP NR511 Week 3 Case Study Part 2 Example
- Loratadine 5mg Tablets. Should take 1 tablet orally once a day.
The patient should resume his loratadine medication because of his seasonal allergic rhinitis which was previously well controlled on this drug together with Fluticasone. Combination of both drugs has been shown to be effective in alleviating symptoms related to allergy.
Patient education
The patient should be educated on general eye care. The patient should be advised against rubbing of the eyes as this causes mast cell degranulation which causes worsening of symptoms. Additionally, educate the patient to avoid exposure to the known allergens. Avoidance of the allergens is the primary modification for all allergic illnesses. This may however not be easy.
Patient should also be educated on the proper application techniques of the eye drops. Application is done by tilting the head backwards and looking up. The lower eyelid should be pulled down to make a pouch where the drop is placed. The patient should wash his hands before applying the drops. He should not touch the dropper. He should replace dropper cap after each use. The patient should also take all medication as prescribed. FNP NR511 Week 3 Case Study Part 2 Example
Referral
Treatment of allergic conjunctivitis might require an interprofessional team led by an ophthalmologist or optometrist.
Active problem list
These are:
- Allergic conjunctivitis
- allergic rhinitis
- Cannabis (marijuana) use
- Alcohol use
I would not make any changes to the treatment plan at this time. I would want to wait and see if the medications are working. Allergic conjunctivitis is best treated with antihistamines and nasal sprays. It is only after evaluating the effectiveness of this plan that I would see if any changes need to be made.
The patient should come back after 4 weeks for follow up. The patient can however comeback earlier if the symptoms do not improve in 2-3 weeks.
FNP NR511 Week 3 Case Study Part 2 Example References
- Dupuis, P., Prokopich, C. L., Hynes, A., & Kim, H. (2020). A contemporary look at allergic conjunctivitis. Allergy, Asthma & Clinical Immunology, 16(1), 1-18. https://doi.org/10.1186/s13223-020-0403-9
Assignment Instructions
Now, assume that any procedures and/or testing which were performed are NORMAL.
1. What is your primary (one) diagnosis for this patient at this time? (support the decision for your diagnosis with pertinent positives and negatives from the case)
2. Identify the corresponding ICD-10 code.
3. Provide a treatment plan for this patient\’s primary diagnosis which includes:
Medication*
Any additional testing necessary for this particular diagnosis*
Patient education
Referral
4. Provide an active problem list for this patient based on the information given in the case.
5. Are there any changes that you would also make to this patient’s overall treatment plan at this time? Must provide an EBM argument for each treatment or testing decision. FNP NR511 Week 3 Case Study Part 2 Example
6. Provide an appropriate F/U plan.
*If part of the plan does not warrant an action, you must explain why. ALL medication and testing decisions (or decisions not to treat with medication or additional testing) MUST be supported with an evidence-based medicine (EBM) argument. Over-the-counter (OTC) and RXs must be written in full as if handing a script to the patient in the office. FNP NR511 Week 3 Case Study Part 2 Example
