NRS 641 Advanced Pathophysiology for Nursing Discussions
NRS 641 Advanced Pathophysiology for Nursing Discussions
NRS 641 Topic 1 DQ 1
What are the differences between primary and secondary line of defense? What factors interfere with these mechanisms? How are these levels of immunity affected in a child, an elderly person, or a person with a chronic disease? Include active, passive, innate, and acquired immunity.
Topic 1 DQ 1 Solution: Primary and Second line of Immunity
Immunity is the ability of the body to prevent the entry of infectious agents and fight the disease-causing micro-organisms. Immunity can either be innate or adaptive. Innate immunity is acquired naturally and forms the primary (first) and secondary (second) line of defense (Günther & Seyfert, 2018). The primary defense is formed by chemical and physical barriers that prevent infections. The physical barriers include intact skin, cilia, and nosocomial bacteria, which prevent the entry of infection. Chemical barriers include mucus, stomach acid, tears, vaginal secretions, and urine flow. On the other hand, secondary defense is formed by white blood cells that fight those pathogens that overcome the primary barriers.
Adaptive immunity protects the body upon re-exposure to the primary pathogens. It is divided into active and passive. T lymphocytes and B lymphocytes are activated to release antibodies that form cell-mediated and immune-mediated immune responses, respectively (Günther & Seyfert, 2018). These responses are part of active immunity that destroys pathogens. In addition, memory cells are formed that aid in fighting the same infections in the future. Finally, in passive immunity, antibodies are created outside the body and can be passed from mother to child during breastfeeding or through the injection of antibodies. Interference in these defensive mechanisms reduces immunity and invasion of the body by infections.
Various factors, including diet, lifestyle, sleep, personal hygiene, genetics, and physical activities, influence the level of immunity (Zimmermann & Curtis, 2019). For instance, physically active individuals, lead a healthy lifestyle, maintain a high level of hygiene, and practice healthy sleeping patterns are likely to have boosted immunity, unlike those who do not. Furthermore, age and general wellbeing also affect immunity. Children have underdeveloped immune responses, whereas the elderly and those with chronic conditions have declined the number of protective cells, leading to reduced immunity. As a result, there is an increased risk of infection due to impaired immunity.
References
Günther, J., & Seyfert, H.-M. (2018). The first line of defense: insights into mechanisms and relevance of phagocytosis in epithelial cells. Seminars in Immunopathology, 40(6), 555–565. https://doi.org/10.1007/s00281-018-0701-1
Zimmermann, P., & Curtis, N. (2019). Factors that influence the immune response to vaccination. Clinical Microbiology Reviews, 32(2). https://doi.org/10.1128/CMR.00084-18
NRS 641 Advanced Pathophysiology for Nursing Discussions DQ 1 Part 2
Choose an inflammatory or infectious process and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical condition can be followed. Include your references in APA style.
DQ 1 Part 2 Solution: Systemic Lupus Erythematous (SLE)
SLE is an autoimmune multi-organ condition characterized by the production of autoantibodies immune complexes that attack the body`s nucleic acids and proteins. The body’s immune system fails to differentiate between its cells and foreign cells resulting in autoantibody formation (Fava & Petri, 2019). The autoantibodies and immune complexes lead to a dysregulated immune response that results in causing inflammation, tissue injuries, pain, and damage. As a result, any organs of the body, including kidneys, heart, skin, lungs, central nervous system, joints, blood, and peripheral nervous system, are affected. Symptoms can either be mild or life-threatening according to the level of tissue involvement.
Unfortunately, the exact cause of immune disturbance remains unknown, but various factors are implicated in etiology. They include genetic predisposition such as HLA gene, hormones including androgen and estrogens, and environmental such as sunlight, chemicals, and sunlight(Fava & Petri, 2019). The immune disturbance leads to suppression of individuals’ immune systems, thus predisposing one to various complications such as life-threatening infections and organ failure.
Prevention of complications and improving patients’ quality of life involves patient education. Education should focus on making the patients understand the nature of the conditions and their effect in compromising the immune status(Navarra et al., 2020). As a result, patients should be educated on medication adherence, frequent medical evaluation for new symptoms, and the need for lipid and sugar monitoring to prevent cardiovascular conditions.
Furthermore, these patients are at increased risk of infection; therefore, they should always check for signs of infection such as fever while seeking early treatment to prevent complications arising from severe infections. Dietary advice includes limiting salt intake, reducing alcohol intake, limiting fat intake while encouraging intake of omega-containing meals and calcium-rich meals. Also, SLE patients should avoid sunlight exposure and ultraviolet light. Finally, they should receive vaccines, quit smoking cigarettes, and plan appropriately for pregnancy.
References
Fava, A., & Petri, M. (2019). Systemic lupus erythematosus: Diagnosis and clinical management. Journal of Autoimmunity, 96, 1–13. https://doi.org/10.1016/j.jaut.2018.11.001
Navarra, S. V., Zamora, L. D., & Collante, M. T. M. (2020). Lupus education for physicians and patients in a resource-limited setting. Clinical Rheumatology, 39(3), 697–702. https://doi.org/10.1007/s10067-019-04795-9
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 1 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 1 DQ 2 Example Answer
Management of SLE
SLE management is guided by patient symptoms and the severity of the conditions. Therefore, various medications, including corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), hydroxychloroquine, and immunosuppressive agents such as azathioprine, are used in flare management. All these medications play various roles in controlling the disease process, including pain and inflammation (Fava & Petri, 2019). However, hydroxychloroquine is widely used for the long-term management of patients with SLE.
Hydroxychloroquine is an antimalarial agent that has properties of disease-modifying anti-rheumatic drugs. It acts using various mechanisms to mediate immunomodulation without overt causing immunosuppression. This is achieved through inhibition of eosinophil chemotaxis and neutrophil locomotion while impairing complement-dependent antigen-antibody reactions (Garg et al., 2021). As a result, it is used to treat constitutional symptoms, arthritis arthralgia, and prevent lupus skin rushes. Furthermore, it reduces mortality and morbidity while avoiding flares. However, hydroxychloroquine monitoring is an integral part of the administration.
Renal and liver functions and retinal examination must be conducted during treatment because it causes toxicity to the liver and kidneys while damaging the retina. In addition, it has other side effects, including diarrhea, angioedema, seizures, ataxia, deafness, liver failure, skin rashes, tinnitus, nausea, and headache. However, complete blood count, creatinine level, and urinalysis should be checked regularly to assess new organ involvement.
Finally, hydroxychloroquine interacts with other medications and should be administered with care. It causes pharmacodynamics antagonism when administered with vaccines such as anthrax, hepatitis A, B, and pneumococcal vaccines, among others, therefore, contraindicated (Garg et al., 2021). Furthermore, it causes QT interval prolongation when administered with albuterol, alfuzosin, amoxapine, and apomorphine; hence, care should be taken. Finally, it causes severe immunosuppression when administered with other immunosuppressive agents such as adalimumab, increasing the risk of infection. Also, over-the-counter medications should be avoided when using hydroxychloroquine to minimize unwanted interactions.
References
Fava, A., & Petri, M. (2019). Systemic lupus erythematosus: Diagnosis and clinical management. Journal of Autoimmunity, 96, 1–13. https://doi.org/10.1016/j.jaut.2018.11.001
Garg, S., Unnithan, R., Hansen, K. E., Costedoat-Chalumeau, N., & Bartels, C. M. (2021). Clinical significance of monitoring hydroxychloroquine levels in patients with systemic lupus erythematosus: A systematic review and meta-analysis. Arthritis Care & Research, 73(5), 707–716. https://doi.org/10.1002/acr.24155
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 2 DQ 1
The Beer\’s criteria contain a list of drugs that are potentially unsafe for use in older persons. Utilize the provided resource, \”American Geriatrics Society 2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults\” for assistance in completing this question. Select a drug on the \”avoid\” list that you have administered to an older patient or a drug that you know is prescribed for an older adult. Relate the outcome of using this drug to the pharmacokinetics (absorption, metabolism, distribution, and excretion) of drugs in an older client. In addition to the link, cite one other reference to support your post. Make sure that you select a different drug than your peers. Include the name of the drug in the subject line so that the drugs can be followed. Include your references in APA style.
Topic 2 DQ 1 Solution
Medications Avoided in Elderly.
Elderly individuals are at increased risk of developing various chronic conditions that require the use of various medications. However, these medications may end up causing more harm than benefit as there is derangement in organ functions in the elderly. Organs such as the liver, kidney, and gastrointestinal are required for absorption, metabolism, distribution, and excretion. Failure in any organ leads to deranged drug function due to pharmacokinetics’ interference. Therefore, to avoid toxicity, the American Geriatric Society provides clear guidelines regarding the prescription of drugs in the elderly to prevent potentially inappropriate medications (PIMs) use as evidenced By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel, (2019).
First-generation antihistamines are anticholinergic drugs listed among other medications as “avoid” in the elderly population. These groups include meclizine, promethazine, chlorpheniramine, clemastine, and doxylamine, among others. They are commonly prescribed to treat rhinitis, insomnia, eczema, pruritus, and conjunctivitis. However, they easily cross the blood-brain barrier and cause major central nervous system side effects, including drowsiness, sedation, fatigue, and cognitive decline (Fein et al., 2019). Furthermore, age advancement causes age-related changes that occur in the cholinergic system; hence there is the risk of decline in cognitive function when anticholinergics are administered. Other anticholinergic effects include constipation, dry mouth, confusion, and blurred vision.
Based on pharmacokinetics, antihistamines are absorbed rapidly, attaining an effective plasma concentration within 3 hours. They undergo hepatic metabolism by cytochrome p450 with potential drug interactions(Fein et al., 2019). Finally, elimination is done by kidneys. Unfortunately, kidney and liver impairment in the elderly increases the risk of toxicity due to impaired metabolism and clearance. Therefore, these medications should be avoided in the elderly population.
References
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. (2019). American Geriatrics Society 2019 updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults: 2019 Ags beers criteria® update expert panel. Journal of the American Geriatrics Society, 67(4), 674–694. https://doi.org/10.1111/jgs.15767
Fein, M. N., Fischer, D. A., O’Keefe, A. W., & Sussman, G. L. (2019). CSACI position statement: Newer generation H1-antihistamines are safer than first-generation H1-antihistamines and should be the first-line antihistamines for treating allergic rhinitis and urticaria. Allergy, Asthma, and Clinical Immunology: Official Journal of the Canadian Society of Allergy and Clinical Immunology, 15(1), 61. https://doi.org/10.1186/s13223-019-0375-9
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 2 DQ 2
Many people are using herbal medications and dietary supplements for the prevention and treatment of medical problems. Review two current research articles about two of these products. Based on the findings, what would be the implications for you as a nurse? What additional research needs to be done in this area? Cite the two references to support your answer. Make sure that you select different herbal medications and dietary supplements than your peers. Include the name of the herbal medication and dietary supplement in the subject line so that the medications can be followed. Include your references in APA style.
Topic 2 DQ 2 Answer
Herbal Medicine and Vitamin supplements.
The use of herbal medication for treatment is increasingly being accepted by most people worldwide. It is estimated that close to 80% of the population uses this product worldwide(Brewer et al., 2019). Furthermore, the advancement in complementary alternative medicine has led to increased use of herbal medicine and supplements. Examples of commonly used herbal medicines include Echinacea, garlic, ginger, ginseng, and turmeric, among others.
The use of these products has shown some recent hope of curing various medical conditions. This has resulted in many patients opting for the same, thus leading to the growth and introduction of these products into markets. However, various public health issues remain regarding safety and potential side effects, and monitoring of their use is limited(Brewer et al., 2019). Furthermore, there is inadequate knowledge about the mode of action, contraindications, and interactions. Therefore, nurses and other healthcare workers should intervene to protect the general population.
Nurses advocate for patient safety and ensure the provision of quality care to patients. Likewise, nurses should be at the forefront of educating populations about the risk of using non-tested or unapproved products for care. Furthermore, nurses can work with various regulatory authorities to ensure that all herbal medications are safe for use with suitable quality(Welz et al., 2018). This can be achieved by ensuring that quality testing and production standards are adhered to before releasing the medication to the general population. In addition, herbal medicines and supplement produce must be licensed to ensure quality. The licensed individuals must understand the information regarding the herbal medicine including indication, use, regulatory information, adverse effects, and safety for use.
Finally, there is need for continuous research regarding herbal medicine. This research should focus on identifying the mode of action, side effects, and molecular components of these products. This will be essential in improving the safety and quality of herbal medicine and herbal supplements.
References
Brewer, N. J., Turrise, S. L., Kim-Godwin, Y. S., & Pond, R. S., Jr. (2019). Nurses’ knowledge and treatment beliefs: Use of complementary and alternative medicine for pain management. Journal of Holistic Nursing: Official Journal of the American Holistic Nurses’ Association, 37(3), 248–259. https://doi.org/10.1177/0898010118822212
Welz, A. N., Emberger-Klein, A., & Menrad, K. (2018). Why people use herbal medicine: insights from a focus-group study in Germany. BMC Complementary and Alternative Medicine, 18(1). https://doi.org/10.1186/s12906-018-2160-6
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 3 DQ 1
Choose a medical condition from the fluid, electrolyte, or acid-base system and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical conditions can be followed. Include your references in APA style.
Topic 3 DQ 1 Example Solution
Fluid, Electrolyte, and Acid-Base Balance: Hyperkalemia.
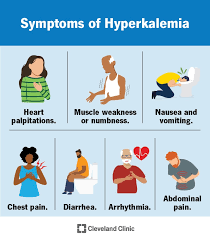
Hyperkalemia is a medical condition characterized by elevated blood potassium levels above 5.0 mmol/L(Jafar et al., 2020). potassium is an important intracellular electrolyte required for the normal function of nerves, heart, and muscles. A disturbance in potassium levels negatively affects the functioning of these systems. This can manifest as muscle weakness, paralysis, numbness, palpitations, tingling, chest pain, and shortness of breath. Notably, potassium levels above 7 cause hemodynamic instability while levels above 8mmol/l lead to respiratory paralysis.
The normal range of potassium is between 3.5- 5.0 mmol/l. (Jafar et al., 2020). The balance of ranges of potassium is dependent on kidney functions and intake. The kidney plays a vital role in the excretion of excess potassium secretion through urination to maintain the balance. Diet, on the other hand, provides the body with potassium to avoid a deficit. The foods rich in potassium include bananas, orange juice, cantaloupe, and honeydew melon. Any dysfunction in kidney function with increased intake of potassium-rich meals creates an imbalance that leads to an increase in serum potassium levels.
Kidney dysfunction can be contributed by various factors including acute and chronic renal failure, drugs, comorbidities, and Addison`s disease (Simon et al., 2022). Kidney failure leads to impairment of excretion function leading to build up potassium and other electrolytes. Furthermore, medications such as amiodarone and spironolactone are potassium-sparing leading to limited excretion by the kidneys. In addition, other medications such as angiotensin-converting enzyme inhibitors and non-steroidal anti-inflammatory drugs can result in hyperkalemia due to a decrease in glomerular filtration rate and aldosterone.
Hypoaldosteronism causes Addison’s disease that further worsens hyperkalemia. Likewise, the presence of commodities such as diabetes type 1 causes derangement in kidney function that leads to hyperkalemia. Finally, intravasation of potassium from extracellular space following serious burns and penetrating trauma can worsen hyperkalemia. All the mentioned process combines to cause non-specific physiologic changes manifesting as hyperkalemia features.
Patient education is an important aspect of patient care. Patients should be informed about the potential causes of hyperkalemia including diet and drugs. Therefore, patients with hyperkalemia should limit their intake of potassium-rich meals and equivalent supplements. Also, they should stop taking medications including potassium-sparring diuretics, NSAIDs, and ACE inhibitors to prevent the risk of hyperkalemia(Simon et al., 2022). Patients should also be taught to check their pulse and identify early features of hyperkalemia for prompt management. Finally, patients should have their potassium levels checked regularly as well as take all prescribed medications appropriately.
References
Jafar, M. S., Thalambedu, N., Kolandra, L., & Roomi, S. (2020). False, reversed but not true: A curious case of hyperkalemia. Cureus, 12(8). https://doi.org/10.7759/cureus.10066
Simon, L. V., Hashmi, M. F., & Farrell, M. W. (2022). Hyperkalemia. https://pubmed.ncbi.nlm.nih.gov/29261936/
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 3 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 3 DQ 2 Sample Approach
Management of hyperkalemia.
Management of hyperkalemia is subject to understanding the cause and severity of the conditions. Treatments are cause-specific aimed at increasing the excretion of potassium. As a result, several treatment modalities are present. The initial care is limiting the oral intake of potassium-rich meals(Khan et al., 2022). Calcium gluconate is used to stabilize the cardiac in the setting of hyperkalemia. Insulin and dextrose are used to shift potassium into cells. Finally, loop diuretics can be used to increase urinary excretion of potassium. Details of furosemide are discussed hereafter.
Furosemide is an example of the loop diuretic used in the management of hyperkalemia. Furosemide causes diuresis through inhibition of the sodium-potassium-2 chloride (Na+-K+-2Cl) co-transporter in the thick ascending loop of Henle and distal convoluted tubule (Khan et al., 2022). Therefore, it is used in conditions associated with water overload. Such conditions include pulmonary edema, congestive heart failure, renal failure, liver failure, and ascites. Its use in the management of hyperkalemia is guided by the principle of inhibiting potassium absorption while increasing its elimination through urine. However, understanding its pharmacodynamics is necessary for monitoring this medication.
Furosemide is through either the oral or intravenous route. However, the dosage is adjusted according to renal functions. Patients with renal dysfunction or kidney failure should receive a lower dosage to lower the risk of toxicity due to a reduction in clearance(Palmer et al., 2021). Therefore, caution should be taken when prescribing medications to people above 65 years. Ototoxicity can also develop more so when administered with ethacrynic acids. Hearing impairment can result from ototoxicity. Hence co-administration with ethacrynic acid is contraindicated. Furthermore, furosemide causes increased water loss and electrolytes leading to dehydration and electrolyte imbalances. Those imbalances include hypomagnesemia, hyponatremia, hypokalemia, and hypocalcemia. Therefore, monitoring of renal functions is essential when taking furosemide. Other adverse effects include diarrhea, anemia, abdominal cramps, anorexia, headache, vertigo, orthostatic hypotension, hyperglycemia, and glycosuria among others.
Finally, furosemide has some drug-drug interactions that must be considered. For instance, ethacrynic acid works with the same mechanism as furosemide leading to serious adverse effects when co-administered, therefore, contraindicated (Palmer et al., 2021). Furthermore, it has pharmacodynamic synergism with some agents including gentamicin, tobramycin, streptomycin, potassium phosphate, and squill. Either of the products increases the effects of the other resulting in worsening adverse effects.
References
Khan, T. M., Patel, R., & Siddiqui, A. H. (2022). Furosemide. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK499921/
Palmer, B. F., Carrero, J. J., Clegg, D. J., Colbert, G. B., Emmett, M., Fishbane, S., Hain, D. J., Lerma, E., Onuigbo, M., Rastogi, A., Roger, S. D., Spinowitz, B. S., & Weir, M. R. (2021). Clinical management of hyperkalemia. Mayo Clinic Proceedings. Mayo Clinic, 96(3), 744–762. https://doi.org/10.1016/j.mayocp.2020.06.014
Topic 4 DQ 1
Choose a medical condition from the respiratory system or HEENT system and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical condition can be followed. Include your references in APA style.
Topic 4 DQ 1 Example Solution
HEENT: Detached Retina
Retinal detachment is a medical condition characterized by separation and pulling of the retina from the retinal pigment epithelium potentially leading to vision loss (Chen et al., 2018). The retina is an internal layer of the eye with numerous nerve vessels that help in image focusing and transmission of information to the brain through the optic nerve to enable vision. Therefore, any dysfunction in the retina leads to interference in visual fields with resultant vision loss. Detachment of the retina also causes deprived oxygen and nourishment supply that can potentially cause nerve cell death and vision loss (Chen et al., 2018). However, other features including darkness, flashlights, reduced vision, and loss of peripheral visual fields may precede visual loss and blindness.
Detachment of the retina is a process culminated by various factors and steps. Causes of detachment can be due to several factors including inflammation, injury, damage, or structural changes. Inflammation causes exudation of fluids with or without a tear to cause increased intraocular pushes that push away the retina to cause detachment. Other causes of exudation leading to detachment include injury to the blood vessels and age-related macular degeneration. Furthermore, injury to the eye or eye surgery can lead to retinal tear that causes accumulation of vitreous gel that pulls the eyeball. This process is termed rhegmatogenous; it is the most common.
In addition, patients with diabetes with poorly controlled blood sugar are predisposed to diabetic retinopathy. Retinopathy causes scarring within the eyeball leading to pushing away of the retina leading to detachment of the retina. This process is called tractional detachment. All these processes integrate risk factors for retinal detachment. Moreover, other risk factors for a detachment include genetics, previous eye surgery, severe myopia, infectious diseases, previous detachment of the eye, pre-eclampsia, cancer of the eye, and trauma.
Finally, patients with retinal detachment are prone to visual problems resulting in visual loss and falls. Therefore, patient education is necessary before or during treatment. First, the patient should be encouraged to increase lighting, remove all hazards, and ask family members to direct them while walking to prevent falls (Kwok et al., 2020). Secondly, patients should not rub their eyes and protect their eyes with eye patches during sleep. Lastly, patients should sleep on either side with an elevated head to help reduce intraocular pressure and reduce the worsening of the retinal detachment. Patients should also adhere to medications as well as be prepared for surgery in case of symptoms worsen.
References
Chen, K.-J., Wang, N.-K., & Wu, W.-C. (2018). Coats disease in a young adult man. JAMA Ophthalmology, 136(12), e183146. https://doi.org/10.1001/jamaophthalmol.2018.3146
Kwok, J. M., Yu, C. W., & Christakis, P. G. (2020). Retinal detachment. Journal de l’Association Medicale Canadienne [Canadian Medical Association Journal], 192(12), E312–E312. https://doi.org/10.1503/cmaj.191337
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 4 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 4 DQ2
Treatment of Retinal Detachment.
Retinal detachment is a medical emergency that requires prompt ophthalmologist review with the initiation of care. Treatment can either be medical or surgical. Surgical treatment is the definitive management upon identification of the course (Bonfiglio et al., 2020). Medical therapy, on the other hand, is auxiliary aimed at relieving symptoms while reducing intraocular pressure. Common medical therapy includes acetazolamide, Tenecteplase, and triamcinolone acetonide. Acetazolamide is discussed hereafter.
Acetazolamide is a diuretic agent classified as a carbonic anhydrase inhibitor. It acts by inhibiting the activities of carbonic anhydrase leading to increased carbonic acid levels(Bonfiglio et al., 2020). Elevated carbonic acid leads to a reduction in body pH with the resultant acidic body. Sodium bicarbonate and chlorides are excreted in an acidic environment with resultant loss of water. As a result, there is increased diuresis that leads to decreased blood pressure, intracranial, and intraocular pressure. Reduction in aqueous humor reduces the risk of retinal detachment and optic nerve. Therefore, this medication can be given either orally or intravenously to reduce intraocular pressure, however, monitoring of side effects is essential.
Acetazolamide causes increased water loss with loss of electrolytes including sodium, sodium bicarbonate, and chlorides. This can result in hyponatremia, hypokalemia, and metabolic acidosis(Farzam & Abdullah, 2022). Therefore, kidney function and blood gases must be evaluated on patients taking acetazolamide. In addition, the administration of acetazolamide leads to reduced clearance of ammonia that increases the risk of hepatic encephalopathy. Unfortunately, patients with kidney and hepatic dysfunction are at an increased rate of encephalopathy, hence monitoring is mandatory. Finally, other common side effects include dizziness, confusion, tinnitus, low libido, paresthesia, black stool, vomiting, nausea, agitation, blurred vision, and abdominal pain. Patients with sulfa allergy may develop Steven Johnson`s syndrome (SJS) by using acetazolamide.
Lastly, acetazolamide interacts with other agents when taken concurrently. For instance, acetazolamide causes increased urine pH that reduces renal clearance of amphetamines thus increasing its toxicity(Liao & Zhu, 2019). Other medications with reduced clearance when administered with acetazolamide include phenytoin, primidone, and quinidine. In contrast, acetazolamide increases the excretion of lithium resulting in reduced efficacy of lithium. Furthermore, there is a risk of kidney stones formation on the administration of acetazolamide with sodium bicarbonate. Finally, the prescription of more than one carbonic anhydrase is discouraged due to the risk of pharmacodynamic synergism that may cause worse adverse effects.
References
Bonfiglio, V., Reibaldi, M., Macchi, I., Fallico, M., Pizzo, C., Patane, C., Russo, A., Longo, A., Pizzo, A., Cillino, G., Cillino, S., Vadalà, M., Rinaldi, M., Rejdak, R., Nowomiejska, K., Toro, M. D., Avitabile, T., & Ortisi, E. (2020). Preoperative, intraoperative, and postoperative corticosteroid use as an adjunctive treatment for rhegmatogenous retinal detachment. Journal of Clinical Medicine, 9(5), 1556. https://doi.org/10.3390/jcm9051556
Farzam, K., & Abdullah, M. (2022). Acetazolamide. https://pubmed.ncbi.nlm.nih.gov/30335315/
Liao, L., & Zhu, X.-H. (2019). Advances in the treatment of rhegmatogenous retinal detachment. International Journal of Ophthalmology, 12(4), 660–667. https://doi.org/10.18240/ijo.2019.04.22
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 5 DQ 1
Choose a medical condition from the cardiovascular system and lymphatic system and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical condition can be followed. Include your references in APA style.
Topic 5 DQ 1 Sample Solution
Cardiovascular and lymphatic system: Arteriovenous Malformations.
Arteriovenous malformations (AVM) are abnormal fistula formation between arteries and veins without a capillary bed (Bokhari & Bokhari, 2021). Arteries functions to pump blood to other parts of the body while veins return the blood to the heart to complete a cycle. Capillaries allow for normal connection between arteries and veins while facilitating oxygen supply and supply of essential nutrients to the body. In AVM abnormal communication interrupts the normal function of arteries, veins, and capillaries. Lack of capillary bed leads to deprived oxygen and nutrients to tissues due to high flow of blood that disrupts nutrient exchange and oxygen (Bokhari & Bokhari, 2021). Hence patients are at risk of low oxygen saturation.
AVMs always occur during early development or shortly after birth. Also, they can occur at any part of the body, however, they are most common in the brain and spinal area (Schimmel et al., 2021). Interestingly, patients may live a normal life without symptoms. Some may be picked incidentally during examination for other pathologies including chronic headaches and seizures. However, they tend to increase in size with time to cause symptoms. Large AVMs are at risk of rupture resulting in severe hemorrhage and hemodynamic instability.
Bleeding to the brain may lead to increased intracranial pressures (ICP). Features of increased ICP include headache, seizures, progressive loss of neurological dysfunction, loss of consciousness, and vomiting. Notably, other risk factors for AVM rupture include prior hemorrhage, deep AVM location, presence of an aneurysm, and exclusive deep venous drainage. In addition, stroke can also develop in the process. Stroke presents with limb weakness, problems in speech, visual problems, and loss of consciousness. Finally, fatal hemorrhage can lead to death.
Finally, patients with AVM should be educated on how t prevent complications. First, patients should adhere to follow-up in the hospital for periodic assessment and early identification of risks of hemorrhage. Secondly, patients should be aware of the deleterious effects of hypertension on AVM (Schimmel et al., 2021). Therefore, patients should avoid strenuous activity and lifting heavy objects to prevent rupture of vessels. Thirdly, patients should not any anticoagulants due to the increased risk of bleeding due to these medications. Finally, patients should be educated about dangerous signs including the neurological deficit, loss of consciousness, repeated seizures, and worsening headache. These signs may require prompt care lest they cause general deterioration.
References
Bokhari, M. R., & Bokhari, S. R. A. (2021). Arteriovenous malformation of the brain. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430744/
Schimmel, K., Ali, M. K., Tan, S. Y., Teng, J., Do, H. M., Steinberg, G. K., Stevenson, D. A., & Spiekerkoetter, E. (2021). Arteriovenous malformations-current understanding of the pathogenesis with implications for treatment. International Journal of Molecular Sciences, 22(16), 9037. https://doi.org/10.3390/ijms22169037
Topic 5 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 5 DQ 2 Example Approach
Management of AVM
AVM management involves complex procedures aimed at correcting the defect and improving patients` quality of life. The mainstay of management is surgery. Radiosurgery and endovascular embolization are common interventional procedures in unstable patients(Gupta & Tripp, 2022). However, there is a role of medical management in stable people using anticonvulsants for seizure control and analgesics for pain management. Phenytoin is the most common anticonvulsant used.
Phenytoin is a hydantoin derivative that controls seizures by blocking voltage-gated sodium channels leading to blockage of the high-frequency repetitive firing of action potentials (Gupta & Tripp, 2022). Inhibition of the repetitive firing leads to slowing down of brain impulses leading to the cessation of seizures. Notably, phenytoin has a wide range of use in controlling generalized seizures with little neurological limit. It can be given orally or intravenously without disruption in its bioavailability. However, dosages should be titrated to avoid potential side effects.
Phenytoin causes various central nervous system side effects. They include drowsiness, confusion, slurred speech, difficulty in balance and coordination, and blurred vision (Kato et al., 2019). These adverse effects individuals` judgment and function, hence should not operate locomotives. In addition, patients can also present with gum swelling, body rashes, chest pain, palpitations, jaundice, and panic attacks while on phenytoin. Sadly, it can penetrate through the placenta to cause teratogenic effects when taken during pregnancy. Therefore, its use during pregnancy should be determined upon evaluation of the risks and benefits.
Various drug-drug interactions exist between phenytoin and other agents. Phenytoin is metabolized by the hepatic enzyme CYP3A4 to its inactive state(Kato et al., 2019). Therefore, it competes with various for the same metabolism pathway leading to antagonism and reduction in the efficacy of various agents. As a result, they are contraindicated. They include ergotamine, lovastatin, lumefantrine, atazanavir, apixaban, tolvaptan, sirolimus, and praziquantel among many others. In contrast, vigabatrin decreases the level of phenytoin levels and reduces efficacy. Finally, a prescription of phenytoin requires the understanding of the other existent interactions. This helps in improving efficacy while reducing side effects.
References
Gupta, M., & Tripp, J. (2022). Phenytoin. https://pubmed.ncbi.nlm.nih.gov/31855364/
Kato, Y., Dong, V. H., Chaddad, F., Takizawa, K., Izumo, T., Fukuda, H., Hara, T., Kikuta, K., Nakai, Y., Endo, T., Kurita, H., Xu, B., Beneš, V., Christian, R., Pavesi, G., Hodaie, M., Sharma, R. K., Agarwal, H., Mohan, K., & Liew, B. S. (2019). Expert Consensus on the management of Brain Arteriovenous Malformations. Asian Journal of Neurosurgery, 14(4), 1074–1081. https://doi.org/10.4103/ajns.AJNS_234_19
Topic 6 DQ 1
Choose a medical condition from the gastrointestinal or genitourinary systems and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical condition can be followed. Include your references in APA style.
Topic 6 DQ 1 Sample Discussion
Genitourinary System: Pyelonephritis.
Pyelonephritis is an infection of the kidneys. The common cause of the infection is gram-negative bacteria with the commonest being Escherichia coli (Belyayeva & Jeong, 2021). Other agents include proteus and klebsiella. In addition, gram-positive bacteria such as Staphylococcus aureus and Enterococci also cause pyelonephritis.
Kidney infections are secondary to infection in other structural organs. Commonly, infections get into the urethra from the anus; from faces. The infectious agent then rises into the bladder which further spreads the infection to the kidneys and collecting ducts (Belyayeva & Jeong, 2021). However, bacteria can also spread through the hematogenous route, though uncommon in healthy individuals but cause more infections in immunocompromised people. Nevertheless, the development of the infection is dependent on both host factors and bacterial virulence.
The ascension of bacteria is favored by urine stasis that allows bacteria attachment aided by adhesins onto the urethral mucosa then spread to cause kidney inflammation and scarring of the renal parenchyma (Sabih & Leslie, 2022). Notably, stasis in urinary flow can be caused by either kidney stones or obstruction along the urethra. Furthermore, bladder outlet obstruction favors an environment that allows the pooling of bacteria and their multiplication. As a result of obstruction, there is reduced urine elimination with resultant reflux of urine into the kidneys to cause inflammation.
The inflammation and scarring of kidneys lead to the presentation of symptomatology. They include flank pain, fever, nausea, burning urination, urgency, vomiting, and increased frequency of urination (Sabih & Leslie, 2022). However, elderly patients may present with advanced features including mental status deterioration, confusion, decompensated organ function, and generalized deterioration that may warrant admission. Consequently, a progressive kidney infection can lead to renal failure, kidney abscess, septic syndrome, septic shock, eventually death. These clinical features define the extent of body reaction to the infectious agent.
The prognosis of pyelonephritis is worse if not identified earlier. Complications such as renal failure and sepsis are life-threatening leading to death. Therefore, early treatment is necessary. However, patients’ education is also an important consideration. Patients must be educated about the potential complications of pyelonephritis. As a result, patients should take their medications as prescribed to prevent antibiotic resistance (Umesha et al., 2018).
Furthermore, patients should take a lot of fluids to avoid dehydration. This is essential because dehydration favors stasis which favors bacterial growth. On the other hand, increased urine flow favors the clearance of micro-organisms hence offering prevention. Finally, female patients should be instructed to practice front-back wiping to prevent the transmission of microorganisms from the anus to the urethra.
References
Belyayeva, M., & Jeong, J. M. (2021). Acute Pyelonephritis. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519537/
Sabih, A., & Leslie, S. W. (2022). Complicated Urinary Tract Infections. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK436013/
Umesha, L., Shivaprasad, S. M., Rajiv, E. N., Kumar, M. M. S., Leelavathy, V., Sreedhara, C. G., & Niranjan, M. R. (2018). Acute pyelonephritis: A single-center experience. Indian Journal of Nephrology, 28(6), 454–461. https://doi.org/10.4103/ijn.IJN_219_16
NRS 641 Advanced Pathophysiology for Nursing Discussions Topic 6 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 6 DQ 2 Example
Management of Pyelonephritis
Treatment of pyelonephritis is complex and is dependent on the stage of patient presentation and patient factors. uncomplicated cases can be managed as an outpatient with oral medications. However, the complicated cases including the severely ill, pregnant women, and those with comorbidities are managed as in-patients using intravenous infusion. Notably, care is aimed at eliminating inflammation using anti-inflammatory as well the elimination of micro-organisms like antibiotics(Chao & Farrah, 2019). However, the choice of antibiotics depends on the result of culture and sensitivity. Finally, surgery also has a role in patients with persistent fevers and deteriorating status despite initiation of medical therapy.
Various antibiotics are used for pyelonephritis management based on the results of the culture. Besides, ciprofloxacin is among the common fluoroquinolones prescribed as first-line for treating infections based on susceptibility. Ciprofloxacin and other fluoroquinolones act by inhibiting enzymes topoisomerase and DNA (deoxyribonucleic acid) gyrase leading to inhibition of cutting and supercoiling of double-stranded DNA required for bacterial cell wall synthesis(Chao & Farrah, 2019). Therefore, they cause defective cell wall synthesis through inhibited DNA synthesis and bacterial growth that results in bactericidal. This agent is effective in suppressing bacterial multiplication that results in pyelonephritis.
Administration of ciprofloxacin should be monitored due to the risk associated with its use. There is a risk of tendinitis and tendon rupture in elderly patients >60 years or the immunocompromised (Gorsane et al., 2018). Liver and function functions must be assessed in patients on this medication. Other side effects include diarrhea, restlessness, arthralgia, headache, abdominal pain, memory loss, allergic reactions, nausea, vomiting, renal calculi, and rushes among others. Therefore, this medication should be taken with care while assessing the adverse effects.
Furthermore, ciprofloxacin exhibits some interactions with other agents based on the pharmacologic and pharmacodynamic properties. Pharmacodynamic antagonism exists when it is administered with BCG and typhoid live vaccine (Umesha et al., 2018). Hence absolute contraindication. Pharmacodynamics exist between ciprofloxacin and tretinoin. On the other hand, it increases the level of flibanserin by inhibiting the enzyme CYP3A4 thus limiting the metabolism of flibanserin (Umesha et al., 2018). However, carbonyl iron and aluminum hydroxide inhibit the absorption of ciprofloxacin in the gastrointestinal leading to decreased levels with resultant low efficacy. These properties require a better understanding of both the pharmacokinetics and pharmacodynamic properties of various agents before administering agents to attain favorable patient outcomes without causing harm.
References
Chao, Y.-S., & Farrah, K. (2019). Fluoroquinolones for the treatment of urinary tract infection: A review of clinical effectiveness, cost-effectiveness, and guidelines. https://www.ncbi.nlm.nih.gov/books/NBK543513/
Gorsane, I., Barrah, S., Barbouch, S., Kaaroud, H., Harzallah, A., & Ben Abdallah, T. (2018). Management of acute pyelonephritis. La Tunisie Medicale, 96(1), 42–47. https://pubmed.ncbi.nlm.nih.gov/30324991/
Umesha, L., Shivaprasad, S. M., Rajiv, E. N., Kumar, M. M. S., Leelavathy, V., Sreedhara, C. G., & Niranjan, M. R. (2018). Acute pyelonephritis: A single-center experience. Indian Journal of Nephrology, 28(6), 454–461. https://doi.org/10.4103/ijn.IJN_219_16
Topic 7 DQ 1
Choose a medical condition from the neurological, musculoskeletal, or integumentary system and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical condition can be followed. Include your references in APA style.
Topic 7DQ 1 Sample Solution
Neurological and musculoskeletal: Locked-in syndrome (LIS)
LIS is a complex neurological disorder caused by lesions that affect the ventral pons and caudal ventral midbrain while sparing the cerebral cortex. These lesions disrupt the neural functioning of the neural that passes through the ventral brainstem. Impairment of brain stem functions leads to paralysis of all voluntary muscles and loss of whole-body sensory while sparing the eye muscles (Das J et al., 2022). As a result, patients with LIS retain some functioning while losing others.
The retain functions include hearing, blinking, vertical eye movement, and cognition with no loss of consciousness. Sparing of pons tegmentum leads to preserved cognition. Interestingly, these patients can hear and reason out but fail to speak. On the other hand, the lost functions include quadriplegia, bulbar palsy leading to dysphagia and anarthria, difficulty in maintaining airway, apnea, vertigo, and hyperpnoea (Das J et al., 2022). Failure to identify the cause and offer early treatment can lead to patient suffering resulting in death.
Various causes are known to cause LIS. They include; brain stem stroke from either hemorrhagic or ischemic stroke; infections such as pseudomonas pontine abscess and meningitis; traumatic brain injury; tumors such as astrocytoma; intracranial bleeding; occlusion of the middle and proximal basilar artery; demyelination caused by central pontine melanosis; multiple sclerosis, and medication overdose (Halan et al., 2021). Any of these abnormalities can impair brainstem functioning leading to debilitating patient function. Therefore, the education of patients and their relatives is paramount to improving functioning.
Patients and caregivers must understand the complexities of LIS and related complications. As a result, basic patient care education should be provided. This includes periodic turning of the patient to prevent bedsores, appropriate feeding techniques using feeding tubes, adherence to prescribed medications, and timely intervention for any signs of worsening condition (Halan et al., 2021). Finally, patients can be trained to use the infrared eye movement sensor for communication with caregivers.
References
Das J, M., Anosike, K., & Asuncion, R. (2022). Locked-in Syndrome. https://pubmed.ncbi.nlm.nih.gov/32644452/
Halan, T., Ortiz, J. F., Reddy, D., Altamimi, A., Ajibowo, A. O., & Fabara, S. P. (2021). Locked-in syndrome: A systematic review of long-term management and prognosis. Cureus, 13(7), e16727. https://doi.org/10.7759/cureus.16727
Topic 7 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 7 DQ 2 Example Paper
Treatment of Locked-in Syndrome.
LIS is a complex neurological condition caused by various etiologies and is characterized by various systemic signs. No single medication has proved to cure LIS. Prompt identification of causative etiology is the mainstay of management. Infections can be treated by antibiotics, tumors can be excised surgically, and the use of neurogenerative compounds in demyelinating causes(Das et al., 2021). However, primary care of maintaining the airway by intubation, maintaining oxygen saturation, and monitoring of circulation is the initial and important step of treatment.
Infections due to meningitis and pseudomonas brain abscess are the most common causes of reversible locked-in syndrome. Ceftriaxone is the most reliable and efficient medication for treating these infections. Ceftriaxone is a third-generation cephalosporin with broad-spectrum coverage. It acts selectively and irreversibly binds to transpeptidases to inhibit the synthesis of the bacterial cell wall (Farr et al., 2021). It penetrates meninges easily and is effective in killing disease-causing bacteria due to the defective cell wall synthesis process.
The pharmacokinetic properties define the effectiveness of the drug. It has low oral bioavailability hence given as an intramuscular or intravenous injection to increase absorption. It is 95% protein-bound with negligible metabolism (Griffiths et al., 2018). Elimination is achieved through kidney excretion in urine and the remainder in feces. Therefore, any derangement in the kidney function limits elimination and favors toxicity which may lead to urolithiasis and post-renal acute renal failure.
Monitoring of side effects is paramount during treatment. The known adverse effects include anemia, jaundice, diarrhea, blood clots, headache, dizziness, Steven-Johnson rash in the allergic patient, and stomach upset. Caution should be taken when administered in neonates as it can worsen hyperbilirubinemia that can result in kernicterus.
Finally, ceftriaxone interacts with other medications leading to serious adverse effects. The use of ceftriaxone and calcium-containing compounds is contraindicated due to the risk of fatal particulate precipitation in the lungs and kidneys (Griffiths et al., 2018). Furthermore, it increases the effects of anticoagulants such as warfarin, heparin, and fondaparinux leading to a decrease in prothrombin time. Last but not least, other antibiotics such as doxycycline, erythromycin, and chloramphenicol causes pharmacodynamic antagonism with ceftriaxone leading to reduced bactericidal effects.
References
Das, J. M., Anosike, K., & Asuncion, R. M. D. (2021). Locked-in Syndrome. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559026/
Farr, E., Altonji, K., & Harvey, R. L. (2021). Locked-in syndrome: Practical rehabilitation management. PM & R: The Journal of Injury, Function, and Rehabilitation, 13(12), 1418–1428. https://doi.org/10.1002/pmrj.12555
Griffiths, M. J., McGill, F., & Solomon, T. (2018). Management of acute meningitis. Clinical Medicine (London, England), 18(2), 164–169. https://doi.org/10.7861/clinmedicine.18-2-164
Topic 8 DQ 1
Choose a medical condition from the endocrine system and explain the pathophysiology changes that may occur. What patient education would need to be included related to this disorder? Make sure that you select a different medical condition than your peers. Include the name of the medical condition in the subject line so that the medical condition can be followed. Include your references in APA style.
Topic 8 DQ 1 Example
Endocrine: Syndrome of Inappropriate Antidiuretic Hormone (SIADH)
SIADH is an endocrine abnormality characterized by continuous and inappropriate secretion of Antidiuretic Hormone (ADH) from the posterior pituitary gland and other sources including lungs due to small-cell lung cancer (Mentrasti et al., 2020). Other causes of SIADH include brain abscess, meningitis, medications such as carbamazepine and amitriptyline, atypical pneumonia, subarachnoid hemorrhage.
Essentially, there is a loss of negative feedback from the hypothalamus to stop ADH release independent of serum osmolality. The excess ADH causes increased reabsorption of water in the distal convoluted tubule with increased urinary sodium loss leading to dilution hyponatremia. The serum sodium levels decrease due to water overload resulting in hyponatremia. The level of hyponatremia determines the clinical manifestation.
Mild hyponatremia presents with acute symptoms such as dizziness and vertigo. In severe hyponatremia, more profound symptoms include loss of consciousness, generalized seizures, cognitive impairment, respiratory distress secondary to brain stem herniation, and other features of hypervolemia including pulmonary edema, increased jugular venous pressure, and ascites (Mentrasti et al., 2020). Prompt identification of symptoms and making an early diagnosis is essential for a better outcome.
People with SIADH are at increased risk of fluid overload with diluted solutes. As a result, patients should be educated about management through restriction of fluid intake (Morris et al., 2018). Reduction in fluid intake reduces fluid overload and corrects sodium levels. Furthermore, patients should be cautioned against rapid correction of hyponatremia as they risk developing central pontine myelinolysis (CMP). Finally, patients should be educated against taking medications such as amitriptyline, selective serotonin receptor inhibitors, and carbamazepine which worsens SIADH.
References
Mentrasti, G., Scortichini, L., Torniai, M., Giampieri, R., Morgese, F., Rinaldi, S., & Berardi, R. (2020). Syndrome of inappropriate antidiuretic hormone secretion (SIADH): Optimal management. Therapeutics and Clinical Risk Management, 16, 663–672. https://doi.org/10.2147/TCRM.S206066
Morris, J. H., Bohm, N. M., Nemecek, B. D., Crawford, R., Kelley, D., Bhasin, B., Nietert, P. J., & Velez, J. C. Q. (2018). The rapidity of correction of hyponatremia due to syndrome of inappropriate secretion of antidiuretic hormone following tolvaptan. American Journal of Kidney Diseases: The Official Journal of the National Kidney Foundation, 71(6), 772–782. https://doi.org/10.1053/j.ajkd.2017.12.002
Topic 8 DQ 2
Select a medication used in evidence-based treatment guidelines for the condition chosen in the first discussion question. Share the mechanism of action of this medication and hints for monitoring, side effects, and drug interactions of which one should be aware. Make sure that you select a different medication than your peers. Include the name of the medication in the subject line so that the medications can be followed. Include your references in APA style.
Topic 8 DQ 2 Sample Solution
Management of SIADH
Treatment of SIADH is non-specific with management tailored towards the etiological process. Therefore, proper identification of etiological process and managing it is the standard care. However, the major goal of treatment is the correction of sodium levels while preventing complications(Bartalis et al., 2021). According to Han et al. (2018), hyponatremia must never be corrected aggressively. The first line of treatment is fluid restriction while the second line is increasing salt intake in combination with loop diuretics and oral sodium chloride. Vasopressin inhibitors such as conivaptan and tolvaptan can be used. Details of conivaptan are discussed hereafter.
Conivaptan is a selective inhibitor of the antidiuretic hormone through inhibiting its V 1A and V2 receptors(Han et al., 2018). This leads to restriction of water absorption at the renal collecting ducts with resultant loss of water through increased urination and subsequent restoration of normal serum sodium concentration. Notably, there is no electrolytes loss in the urine. It is indicated for the treatment of euvolemic and hypervolemic hypernatremia. Mostly given in hospital set-up through the intravascular route infused with normal saline. However, it should not be prescribed in people with known allergies to the product or those who can not pass urine.
Conivaptan has various known side effects that require monitoring. To begin with, conivaptan causes irregularities in potassium levels. It can lead to hypokalemia. As a result, doing serial kidney function tests is necessary during treatment. Features of hypokalemia include muscle weakness, muscle spasms, palpitations, fatigue, numbness, difficulty in breathing, changes in mood, and problems with digestions including diarrhea and constipation (Han et al., 2018).
Other side effects include headache, nausea, vomiting, troubles in sleeping, thirst, dehydration, dry mouth, anemia, confusion, pruritus, pneumonia, and injection site reaction including pain, erythema, and fever. in addition, due to increased water loss, this medication can lead to orthostatic hypotension. Therefore, patients on conivaptan should be warned against rapid rise from a lying or a sitting position to prevent falls that may cause trauma. in addition, if signs of hypovolemia or hypotension persist, the medication should be stopped and a complete reassessment is done. Finally, rapid correction of hyponatremia leads to CMP.
Features of CMP include dysphagia, mutism, dysarthria, seizures, coma, spastic quadriparesis, lethargy, and affective changes. Therefore, care should be taken when prescribing and using conivaptan due to serious death effects. Prescription alongside other agents should also be cautious due to interactions with other products.
Conivaptan has various levels of interactions ranging from minor to severe with other agents. Therefore, there are contraindications to prescription with other agents while others cause serious reactions. Conivaptan is contraindicated to be used with medications metabolized by CYP3A4 because it inhibits the enzyme CYP3A4 leading to an increase in the concentration of medications metabolized by CYPP3A4 (Bartalis et al., 2021).
Examples of such medications include lopinavir, indinavir, isoniazid, chloramphenicol, clarithromycin, ergonovine, imatinib, and ketoconazole among others. Yet other serious effects can be seen when conivaptan is prescribed with amitriptyline, apomorphine, amlodipine, apixaban, bromocriptine, and carbamazepine. An alternative may be used or other medications should be stopped while using conivaptan to prevent serious drug interactions.
References
Bartalis, E., Gergics, M., Tinusz, B., Földi, M., Kiss, S., Németh, D., Solymár, M., Szakács, Z., Hegyi, P., Mezösi, E., & Bajnok, L. (2021). Prevalence and prognostic significance of hyponatremia in patients with lung cancer: Systematic review and meta-analysis. Frontiers in Medicine, 8, 671951. https://doi.org/10.3389/fmed.2021.671951
Han, S. W., Yi, J. H., Kang, K. P., Kim, H. Y., Kim, S. W., Choi, H. Y., Ha, S.-K., Kim, G.-H., Kim, Y. W., Jeong, K. H., Shin, S. K., & Kim, H.-J. (2018). Safety and efficacy of tolvaptan in Korean patients with hyponatremia caused by the syndrome of inappropriate antidiuretic hormone. Journal of Korean Medical Science, 33(15). https://doi.org/10.3346/jkms.2018.33.e112
Also Read: GCU NUR-665E Nursing Education Practicum Discussion Questions
