Quality Safety and Cost Considerations NURS-FPX4900 Assessment 2
Assessment 2: Assessing the Problem: Quality, Safety, and Cost Considerations Instructions
- In a 5-7 page written assessment, assess the effect of the patient, family, or population problem you’ve previously defined on the quality of care, patient safety, and costs to the system and individual. Plan to spend approximately 2 direct practicum hours exploring these aspects of the problem with the patient, family, or group you’ve chosen to work with and, if desired, consulting with subject matter and industry experts.
- Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form. Report on your experiences during your first two practicum hours.
Instructions
Complete this assessment in two parts.
Part 1
Assess the effect of the patient, family, or population problem you defined in the previous assessment on the quality of care, patient safety, and costs to the system and individual. Plan to spend at least 2 practicum hours exploring these aspects of the problem with the patient, family, or group. During this time, you may also consult with subject matter and industry experts of your choice. Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form. Use the Practicum Focus Sheet: Assessment 2 [PDF] provided for this assessment to guide your work and interpersonal interactions.
Part 2
Report on your experiences during your first 2 practicum hours, including how you presented your ideas about the health problem to the patient, family, or group.
-
- Whom did you meet with?
- What did you learn from them?
- Comment on the evidence-based practice (EBP) documents or websites you reviewed.
- What did you learn from that review?
- Share the process and experience of exploring the influence of leadership, collaboration, communication, change management, and policy on the problem.
- What barriers, if any, did you encounter when presenting the problem to the patient, family, or group?
- Did the patient, family, or group agree with you about the presence of the problem and its significance and relevance?
- What leadership, communication, collaboration, or change management skills did you employ during your interactions to overcome these barriers or change the patient’s, family’s, or group’s thinking about the problem (for example, creating a sense of urgency based on data or policy requirements)?
- What changes, if any, did you make to your definition of the problem, based on your discussions?
- What might you have done differently?
- What barriers, if any, did you encounter when presenting the problem to the patient, family, or group?
- Whom did you meet with?
Quality Safety and Cost Considerations NURS-FPX4900 Requirements
The assessment requirements, outlined below, correspond to the scoring guide criteria, so be sure to address each main point. Read the performance-level descriptions for each criterion to see how your work will be assessed. In addition, note the additional requirements for document format and length and for supporting evidence.
-
- Explain how the patient, family, or population problem impacts the quality of care, patient safety, and costs to the system and individual.
- Cite evidence that supports the stated impact.
- Note whether the supporting evidence is consistent with what you see in your nursing practice.
- Explain how state board nursing practice standards and/or organizational or governmental policies can affect the problem’s impact on the quality of care, patient safety, and costs to the system and individual.
- Describe research that has tested the effectiveness of these standards and/or policies in addressing care quality, patient safety, and costs to the system and individual.
- Explain how these standards and/or policies will guide your actions in addressing care quality, patient safety, and costs to the system and individual.
- Describe the effects of local, state, and federal policies or legislation on your nursing scope of practice, within the context of care quality, patient safety, and cost to the system and individual.
- Propose strategies to improve the quality of care, enhance patient safety, and reduce costs to the system and individual.
- Discuss research on the effectiveness of these strategies in addressing care quality, patient safety, and costs to the system and individual.
- Identify relevant and available sources of benchmark data on care quality, patient safety, and costs to the system and individual.
- Document the time spent (your practicum hours) with these individuals or group in the Capella Academic Portal Volunteer Experience Form.
- Use paraphrasing and summarization to represent ideas from external sources.
- Apply APA style and formatting to scholarly writing.
- Explain how the patient, family, or population problem impacts the quality of care, patient safety, and costs to the system and individual.
Additional Requirements
-
- Format: Format your paper using APA style. APA Style Paper Tutorial [DOCX] is provided to help you in writing and formatting your paper. Be sure to include:
- A title page and reference page. An abstract is not required.
- Appropriate section headings.
- Length: Your paper should be approximately 5–7 pages in length, not including the reference page.
- Supporting evidence: Cite at least 5 sources of scholarly or professional evidence that support your central ideas. Resources should be no more than five years old. Provide in-text citations and references in APA format.
- Proofreading: Proofread your paper, before you submit it, to minimize errors that could distract readers and make it more difficult for them to focus on its substance.
- Format: Format your paper using APA style. APA Style Paper Tutorial [DOCX] is provided to help you in writing and formatting your paper. Be sure to include:
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
-
- Competency 3: Transform processes to improve quality, enhance patient safety, and reduce the cost of care.
- Explain how a patient, family, or population problem impacts the quality of care, patient safety, and costs to the system and individual.
- Propose strategies to improve the quality of care, enhance patient safety, and reduce costs to the system and individual and document the practicum hours spent with these individuals or group in the Capella Academic Portal Volunteer Experience Form.
- Competency 5: Analyze the impact of health policy on quality and cost of care.
- Explain how state board nursing practice standards and/or organizational or governmental policies can affect a patient, family, or population problem’s impact on the quality of care, patient safety, and costs to the system and individual.
- Competency 8: Integrate professional standards and values into practice.
- Use paraphrasing and summarization to represent ideas from external sources.
- Apply APA style and formatting to scholarly writing.
- Competency 3: Transform processes to improve quality, enhance patient safety, and reduce the cost of care.
Quality Safety and Cost Considerations NURS-FPX4900 Example
Obesity is a non-communicable disease and a leading cause of morbidity and mortality across various health populations in the US. Among the most affected populations is the African Americans. As justified in the previous assessment, adult and childhood obesity is a health problem that needs consideration. Being one of the minority populations, African Americans needs extra emphasis, mainly because obesity in this population is known to have contributed to the high prevalence of other chronic illnesses such as diabetes mellitus.
Obesity is costly and exerts considerable financial pressure on the individual, their family, and the healthcare system. It also impacts the quality of care and patient safety. The government and the health sector play a massive role in the quality of care, patient safety, and costs for obesity among African American patients. This paper will focus on the impact of the population problem on the quality of care, patient safety, and cost, how the state board of nursing affects the population’s impact on care quality, patient safety, and cost, and after that, propose strategies to improve the quality of care, enhance patient safety and reduce costs to the system and individuals.
Impact of Obesity Among African Americans on Care Quality, Patient Safety, and Costs to the System and Individuals
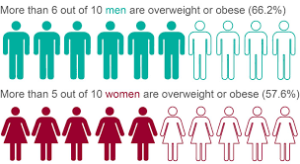
African Americans have the highest age-adjusted prevalence of obesity among other health populations in the US, with 49.9% of adults being obese (CDC.gov, n.d.). The high prevalence indicates that this population needs obesity healthcare attention greatly. However, it is a minority group that faces health inequalities; thus, the quality of care may be low. Treating and managing obesity is complex due to its complex nature.
According to Cardel, Jastreboff & Kelly (2019), the choice of treatment is also based on the patients’ age, psychosocial factors, comorbidities, and the severity of obesity. More so, obesity treatment is supposed to be a continuum of care, beginning with the less invasive. All treatment options should be discussed with the family, and an appropriate care plan developed based on the patients’ needs.
Common treatment options include behavioral interventions, bariatric surgery, and pharmacotherapy. However, some of the interventions’ safety and efficacy are inadequate or lack enough evidence (Cardel et a., 2019). For instance, the risk of bariatric surgeries may include specific malnutrition deficiencies. There is also a shortage of obesity medicine specialists. Therefore, the quality of care and patient safety of obese patients is compromised, especially in underserved populations. Inadequate specialists prevent good care delivery since one care provider is expected to serve a large population.
It may compromise patient safety and put individuals at risk of patient safety issues such as medication errors. Patient safety and quality issues also impact the healthcare system. They may lead to readmissions and hospital-acquired infections, adversely affecting the patients and the system. In addition, issues such as stigmatization and weight bias faced by obese patients by some healthcare providers may negatively affect the patient and contribute to patient safety issues.
The problem of obesity among African Americans also impacts the cost to the system and the individuals. CDC.gov (n.d.) notes that the annual estimated medical cost of obesity is about $173 billion. The medical costs and expenses of obese patients are $1861 higher than those of people with a healthy weight. The percentage of healthcare costs associated with obesity is rising, not forgetting the economic impact of obesity on the individual, the family, and the nation.
A study by Biener, Cawley & Meyerhoefer (2018) established that obesity negatively affects economic outcomes such as wages, employment, and medical care costs, imposing external expenses that may require government interventions. Obesity also raises individuals’ healthcare costs considerably. Obesity affects earnings and wages since an obese person is likely to be less productive than people with a healthy weight.
Obese individuals may also be disqualified from employment opportunities that require physically fit individuals. The global economy also suffers decreased productivity due to the workforce reduction caused by obesity and its related illnesses that may force people not to work (Beiner et a., 2018).
In addition, obesity may contribute to other chronic illnesses such as type 2 diabetes, stroke, cancer, and cardiovascular conditions, thus escalating healthcare costs and posing a financial burden to the individual and the family. Some family members may be affected excessively by their patients’ cost burdens and neglect. The neglected patients exert considerable financial pressure on the healthcare system and the government. Prevention and effective management of obesity can improve care quality, enhance the quality of life and reduce costs to the individual, their families, and the healthcare system.
Nursing Practice Standards and or Organizational or Governmental Policies Effects on African American Population with Obesity
The local state and federal governments and other non-governmental organizations significantly ensure quality care, patient safety, and cost containment for all underserved populations with obesity. The government can influence the quality of care, patient safety, and costs of obesity to the individuals and the system by developing policies to prevent obesity and improving access to obesity help services by making them affordable.
For instance, policies to prevent obsity and encourage healthy lifestyles can include encouraging increased physical activity, improving nutrition, and encouraging mobility. Trust for Americas Health is one organization that strives to promote health and fight for individuals with obesity, with a particular focus on minority populations. It has advocated for policies such as healthier food packages and unhealthy beverage taxes to reduce obesity.
It also advocates for federal best practices to build state and local capacity and reduce disparities. It recommends the expansion of the CDCs State Physical Activity and Nutrition (SPAN) program, increasing funding for the Racial and Ethnic Approaches to Community Health (REACH) program, and creation of grant programs that will address social determinants of health across all health populations (Trust for Americans Health.org, 2019).
Government policies also ensure affordability and accessibility of care, promoting disease prevention interventions and subsidizing healthcare costs. It encourages obese patients to seek medical attention in healthcare institutions, hence healthcare access and care quality. However, most minority populations, such as African Americans, still do not access obesity care effectively. The government has been proactive in obesity prevention interventions, thus promoting care quality and safety.
Government policies significantly impact nurses’ intervention in promoting health and wellness for African Americans with obesity. A nurse should be able to recognize marginalized populations and provide interventions that best suit their needs. However, the interventions must be in line with the policy stipulations of the state of practice and the scope of practice that the nurse is allowed to practice in that particular state.
The state government regulates the nurses’ scope of practice through the nursing practice act under the state board of nursing. The two define the roles and scope of practice regarding obesity treatment and management. The nursing practice act stipulations require nurses to provide affordable, high-quality, and safe care to all patients (Cassiani et al., 2020). Nurses must thus provide ethically acceptable interventions and relay no harm to the individuals within the nursing scope of practice as stipulated by these policies and regulations at the local, state, and national levels.
Proposed Strategies to Manage Obesity among African American Population
Various strategies are required to improve the quality of care, enhance patient safety and reduce the cost of managing obesity among African Americans. The first strategy is dealing with weight stigma as a psychosocial factor in obesity-focused prevention and treatment (Puhl, Himmelstein & Pearl, 2020).
Weight stigma and weight bias are the most significant barriers to implementing current evidence-based practices to manage obesity. African Americans specifically face more weight bias due to being a minority population. Effective management of obesity in this population will require refocusing on weight bias among healthcare providers and society. Dealing with weight stigma will encourage more obese patients to seek medical help, thus increasing access to services and improving patient outcomes.
Furthermore, the government can introduce affordable health insurance to this minority population to afford obesity care. Obesity treatment is costly, and most African Americans cannot afford it and thus shy away from seeking medical help. There is private and public insurance that helps citizens afford healthcare costs. However, not all citizens, especially minorities such as African Americans, afford the insurance. The government should ensure insurance acts such as Medicaid are affordable for even the low-class citizens at a higher risk, with a higher prevalence of obesity.
Conclusion
Obesity negatively affects the African American population. The quality of care this population receives is altered by inadequate access to care, the high cost of managing the condition, as well as weight stigmatization, and weight bias. The high costs of treatment and management of obesity pose a considerable burden to individuals, their families, and the healthcare system. Hence, there is a need for formidable strategies to ensure cost containment, high-quality care delivery, and patient safety. Prevention education and the introduction of affordable insurance are effective strategies, as discussed above.
Quality Safety and Cost Considerations NURS-FPX4900 References
Biener, A., Cawley, J., & Meyerhoefer, C. (2018). The impact of obesity on medical care costs and labor market outcomes in the US. Clinical Chemistry, 64(1), 108-117. https://doi.org/10.1373/clinchem.2017.272450
Cardel, M. I., Jastreboff, A. M., & Kelly, A. S. (2019). Treatment of Adolescent Obesity in 2020. JAMA, 322(17), 1707. https://doi.org/10.1001/jama.2019.14725
Cassiani, S. H. D. B., Lecorps, K., Cañaveral, L. K. R., da Silva, F. A. M., & Fitzgerald, J. (2020). Regulation of nursing practice in the Region of the Americas. Pan American Journal of Public Health, 44. https://dx.doi.org/10.26633/RPSP.2020.93
Puhl, R. M., Himmelstein, M. S., & Pearl, R. L. (2020). Weight stigma as a psychosocial contributor to obesity. American Psychologist, 75(2), 274. https://psycnet.apa.org/doi/10.1037/amp0000538
The Center for Disease Control and Prevention (n.d.). Adult Obesity Facts. https://www.cdc.gov/obesity/index.html
Trust for Americans Health.org. (n.d.). The state of obesity: better policies for a healthier America. With Special Feature on Racial and Ethnic Disparities in Obesity and Advancing Health Equity. https://www.tfah.org/wp-content/uploads/2019/09/2019ObesityReportFINAL-1.pdf
Also Read: NURS-FPX4030 Assessment 1
