Root Cause Analysis and FMEA Process Example Paper
Part A
Introduction: Meaning of Root Cause Analysis-RCA
Root cause analysis is a tool used by healthcare organizations to effectively study adverse events/incidences that cause patient harm within a healthcare facility. RCA in healthcare organizations is a critical tool used to analyze where adverse events/outcomes or patient harm occurred to identify and address their root cause (Caselli et al., 2018). Understanding RCA helps healthcare facilities to emphasize patient safety by preventing potential future harm. An effective RCA allows healthcare organizations to design and implement effective solutions that address failures at their sources.
RCA Step 1: Create a Multi-Disciplinary Team
Implementation of interventions is a critical part of quality care in healthcare. Root cause analysis is a method that identifies errors and incidences with a view of taking appropriate corrective measures. These corrective measures lead to change in strategies that ultimately result in the improvement in quality (Cherry, & Jacob, 2017). The strategies used in managing change determine how successful the implementation of change will be.
The first step in RCA is formulating a multidisciplinary team to analyze the adverse events/incidence. The team should be composed of different health interprofessional within the healthcare facility. This team looks at what happened, how it happened and proposes effective action as remedies for the event/incident.
RCA Step 2: Identifying what Happened
Mr. B, a 67-year old man was brought to the hospital complaining of severe pain in his left leg and the hip area. The patient got this pain after losing his balance while avoiding stepping on his dog, he tripped and fell. At the hospital, Mr. Bs vitals were recorded as follows: B/P 120/80, HR-88 (regular), T-98.6, and R-32, and his weight was recorded at 175 pounds.
However, Mr. continued to moan on his hip area and left leg and rates his pain as 10 over 10. The attending nurse, Nurse J. finds that Mr. B suffers from the problem of glucose impairment. Mr. Bs last visit to a hospital shows elevated levels of lipids and cholesterol. Besides, Mr. Bs current medication includes atorvastatin and oxycodone for his chronic back pain.
To deal with Mr. Bs pain, Dr. T instructs Nurse J to give Mr. B 5mg IVP diazepam which is administered at 4.05 pm. After five minutes without any visible effect of the drug, Dr. T instructs Nurse J to give the patient another medication-2mg IVP hydromorphone which is administered at 4.15 pm. After five minutes of administering 2mg IVP hydromorphone, Dr. T still feels unsatisfied with the sedation effort.
He-the doctor, again instructs Nurse J to give another dosage of 2 mg hydromorphone IVP and another additional 5mg diazepam IVP. Dr. T’s goal is to have complete relaxation of the patient’s skeletal muscle to manually relocate and align the patient’s hip. At 4.25 pm., Mr. B appears sedates and his left hip is successfully adjusted/aligned. Throughout this process, the patient remains sedated and is left to sleep off the sedatives. He is not put on supplemental oxygen.
RCA Step 3: Analyzing what should Have Happened
To begin with, Mr. B should have been placed on an electrocardiogram-EKG considering his elevated blood pressure based on the records of his last hospital visit a few days ago. The EKG would have picked any irregularities/abnormalities such as palpitations on Mr. B’s heart/vital signs. Secondly, the nurse should have actively monitored Mr. B’s oxygen level frequently.
At some point, Mr. B’s O2 saturation alarm goes off when his O2 level drops to 85%. The attending LPN enters the room and resets the alarm and repeats the blood pressure reading, but does not put the patient on supplemental oxygen. Third, the number of sedatives given to Mr. B was too much for his body to take leading to a cardiac arrest.
RCA Step 4: The Root Cause
This is the step where the RCA team analyzes what happened by asking why. In Mr. B’s case, several adverse events led to his eventual death. The contributing adverse events in this case included; shortage of personnel, sedation issue, oxygen issue, and excessive sedation. On staffing, this rural hospital has an emergency department with six rooms but with only two nurses-one RN and an LPN. These two nurses had to attend to patients other than Mr. B. Had the facility had enough staff, there would have been a clinician attending to Mr. round the clock.
Secondly, Dr. T gave the patient two different sedatives in quick succession leading to respiratory depression. Third, between 4.35 pm and 4.40 pm, the LPN comes back to Mr. B’s room after his B/P alarm went off. At this point, the patient’s O2 saturation level was 85% but the LPN did not do anything about it. He/she simply reset Mr. B’s B/P alarm and went away.
RCA Step 5: Developing Causal Statements
Dr. T did not take into account the patient’s history before administering the sedatives to him. The LPN erred by not putting the patient on supplemental oxygen when his O2 saturation level went off. Nurse J did not provide Mr. B with adequate attention due to her busy schedule being the only RN in the facility. The lack of oxygen was the biggest contributing factor to the brain death of Mr. B.
RCA Step 6: Take Action
The facility must hire enough LPN’s and RN’s that resonate with their patient traffic. Lack of adequate personnel led to Mr. B being abandoned/neglected as the LPN and the RN attended to other patients. Training and re-training nurses/clinicians on early warning systems. This will help them to identify potential problems early. Staff members must be retrained to make them aware of the importance of supplemental oxygen to sedated patients. The facility must adopt an effective clinical practice guideline emphasizing frequent monitoring and observation of sedated patients.
Part B: Propose a Process Improvement Plan
Root Cause Analysis supports the continuous improvement process because they uncover the underlying causes of problems in healthcare which are used by organizations to implement improvement efforts. As Gesser-Edelsburg et al. (2018) notes, RCA helps organizations to assess identified errors or incidences and differentiate between latent and active errors. After the identification of incidences/errors, organizations make necessary changes that maximize efficiency, improve quality of care, and improve the organizational environment while enhancing patient outcomes.
Lewin’s change theory could be applied to the proposed improvement plan by identifying the areas of strengths and weaknesses. In this case study, the organization can use Lewin’s change management to point out the weaknesses/lapse and strengths of its personnel and take corrective measures where need be. Additionally, Lewin’s change management approach helps organizations to reduce resistance to change by employees.
Part C: Failure Mode and Effects Analysis (FMEA) Process.
Failure Mode and Effect Analysis-FMEA refers to the identification of potential failures and the effects of such failures on patients, nurses, and healthcare facilities. In this approach, healthcare facilities use data/information to prioritize failures/adverse incidences based on their consequences and impact.
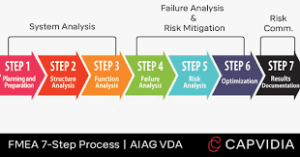
Steps of FMEA
Step 1: Process selection- This is where the process to be analyzed is selected. Here, a problem is identified for analysis.
Step 2: Selection of Staff- At this stage, an organization puts in place a team to work on the FMEA. The team is drawn from the staff members directly affected/impacted by the process being analyzed.
Step 3: Process description-Here, the process being analyzed is clearly defined so that team members know exactly what they are dealing with. Using flowcharts can create a clear picture of what is being done.
Step 4: This step involves the identification of potential problems during the stages of the process. After identification of potential problems, the team must come up with solutions to these problems.
Step 5: prioritize problems. At this stage, the team must eliminate problems using probability. For example, problems are eliminated based on their probability to reoccur and their severity.
Step 6: Here, an organization must design and implement changes. Simply put, this is the stage concerned with the interventions used to prevent or reduce or eliminate problems/failures.
Step 7: This step is about measuring the changes implemented to evaluate their effectiveness.
Part D: Testing Intervention
Testing the effectiveness of the adopted interventions requires a frequent review of the FMEA. A process improvement plan-PIP is a critical tool that can be used to test the intervention. The PIP measures what is working and what is not and continuously replacing what is not working with new measures even as the implementation continues (Cherry, & Jacob, 2017). For example, in this case, study, clinicians should institute professional collaboration amongst them to discuss matters.
Part E: Nursing Leadership
Nurses should actively participate in FMEA and RCA processes because they spend a lot of time with patients. Using these two critical tools helps nurses to adopt a patient-centered approach in dealing with patients. Patient-centered care leads to better patient outcomes, patient satisfaction, and improved quality care.
Leadership is important in every organization because it defines the level of success in every organization. The facility must adopt effective leadership and communication strategies to fulfill the organization’s goals and objectives. The organization requires other leadership tools such as intranets and other chat programs. programs such as live chat systems, video conferencing allow staff to effectively collaborate. All these leadership tools and systems will ensure speedy and efficient leadership between employees themselves and leadership between employees and the management of the organization. Some of these leadership systems are simple and cheap and yet very effective in providing leadership solutions.
Root Cause Analysis and FMEA Process Example Paper References
- Caselli, E., Brusaferro, S., Coccagna, M., Arnoldo, L., Berloco, F., Antonioli, P., Tarricone, R., Pelissero, G., Nola, S., La Fauci, V., Conte, A., Tognon, L., Villone, G., Trua, N., Mazzacane, S. & Conly, J. (2018). Reducing healthcare-associated infections incidence by a probiotic-based sanitation system: A multicentre, prospective, intervention study. PLOS ONE, 13(7), e0199616–. doi:10.1371/journal.pone.0199616.
- Cherry, B., & Jacob, S. R. (2017). Contemporary nursing: Issues, trends, & management. Elsevier Health Sciences. doi:10.1114/13756-018-0418
- Gesser-Edelsburg, A., Cohen, R., Halavi, A. M., Zemach, M., van Heerden, P. V., Sviri, S., Benenson, S., Trahtemberg, U., Orenbuch-Harroch, E., Lowenstein, L., Shteinberg, D., Salmon, A. & Moses, A. (2018). Beyond the hospital infection control guidelines: a qualitative study using positive deviance to characterize gray areas and to achieve efficacy and clarity in the prevention of healthcare-associated infections. Antimicrobial Resistance & Infection Control, 7(1), 124–. doi:10.1186/s13756-018-0418-x https://aricjournal.biomedcentral.com/
Also Read: Safe Nurse Patient Ratios and Acuity Based Staffing Paper
