NURS FPX6011 SimmonsC Assessment 1 Evidence-Based Patient-Centered Concept Map Example
Assessment Case Study: Evidence-Based Patient-Centered Concept Map
Carol Lund Case Study
The patient in this case study had a delivery 10 weeks ago through cesarean section delivery. She was diagnosed with gestational diabetes at 30 weeks and was to be started on insulin as his obstetrician advised. However, the patient’s family and cultural beliefs did not agree with this practice because they argued that the insulin to be used was from nonhumans or synthesized in the lab.
Her only mode of treatment is dietary control and exercise, but her recent schedule does not allow her to manage these self-interventions. She checks her blood glucose randomly and after the meals, but it is still persistently high ten weeks after delivery despite her obstetrician telling her that they would normalize. This patient exhibits various needs that may benefit from nursing interventions.
Information and Educational Needs
The patient exhibits patient educational and emotional needs as well as needs to stabilize her blood glucose levels. She exhibits unstable plasma glucose levels, deficient knowledge of gestational diabetes, dietary and nutritional needs, and emotional stress. These needs have been arranged in order to prioritize this patient. In gestational diabetes, the blood glucose levels usually return to normal after six weeks postpartum.
Most patients get gestational diabetes mellitus during the third trimester, but their insensitivity and blood glucose return to normal (Plows et al., 2018). However, about 15% of these women do not achieve normal glycemic control by the eighth week postpartum (Kautzky-Willer et al., 2019). Carol Lund, the patient in this case scenario, did not achieve normal glycemic control after the postpartum control. She develops persistently high blood glucose levels that place her at risk of various complications such as type II diabetes, infections, dehydration, and cardiovascular, and renal diseases (Gomes et al., 2018). Therefore, there is a need to maintain her blood glucose levels within the normal limits and stabilize them.
Patient and Family’s Knowledge Needs
The patient demonstrated deficient knowledge regarding the treatment and outcomes of her gestational diabetes. Addressing patient information and education needs improves the overall quality of care (Blount, 2020). Awareness and knowledge of GDM are improving patients’ uptake of treatment interventions, thus good patient outcomes (Brown et al., 2018). In Carol’s case, family and cultural beliefs have largely influenced her uptake of GDM treatment.
As such, she does not take insulin, owing to the belief that it came from animals or was manufactured in the lab somewhere. Fortunately, she believes that insulin is not the only option for her treatment. A study by (Prabhu et al., 2021) found that less than half of reproductive women were unaware of gestational diabetes complications and about half were aware of the existence of gestational diabetes mellitus. According to this study, patient education was significantly associated with knowledge scores. The provision of scientific health facts to this patient could influence her health literacy and decision-making.
Emotional Needs
Emotional needs also form a part of patient-centered. Without addressing the patient’s emotional concerns, their patient experience and satisfaction are not guaranteed (Liang, 2022). Carol has also expressed her anxiety about the possibility of diabetes in her child in the future. Her fears are based on the belief that her GDM is genetic and thus transmissible between generations.
She needs to understand that diabetes mellitus is largely a lifestyle disease and conditions such as obesity and overweight are key risk factors. However, she must also understand that the risk of type II diabetes mellitus is sevenfold in her following her gestational diabetes mellitus (Kautzky-Willer et al., 2019). Her emotional needs are related to her cultural beliefs, health literacy, and activities of daily living schedule.
Value and Relevance of Evidence Used as the Basis of Patient-Centered Concept Map
The analysis of the needs and development of this patient’s patient-centered concept map has been guided by evidence from credible literature. Three articles and three books on nursing practice have been used. These studies were published by credible authors who have good expertise and command in the respective fields. These articles are scholarly and were peer-reviewed. They were sourced from credible journals such as PubMed and Scopus.
These sources of evidence provided scientific reasoning behind the patient’s needs. The provided scientific proof that the problems that this patient was facing are existent and have been reported through literature. The pathobiology of GDM, the existence of deficiency of patient knowledge about GDM, and the outcomes and treatment modalities of GDM are well explained in these litteratrice items. The articles provided different levels of literature, including review, cohort, and cross-sectional studies. The evidence was published in the last five years and is thus current and relevant to the current practice.
Proposed Criteria for Patient Outcome Evaluation
Addressing these patient needs should result in holistic patient care outcomes. Spiritual, mental, emotional, and physical health outcomes would describe the quality of the care provided. The major interventions in the concept map were patient education and monitoring. These two interventions would help the patient makes healthy decision toward achieving holistic health, including stable glycemic control.
To evaluate the outcomes of her health, a serial assessment of her blood glucose, patient experience, and quality of glycemic control will provide a picture of the effectiveness of the interventions. Objective assessment of the patient experience through feedback after the care, A1c measurements, and objective assessment of signs and symptoms of complications are the specific items that would be evaluated to provide measures of success. These criteria are useful and appropriate because they assess the quality as well as the safety of the care provided.
Patient and Family Communication Plan
My communication plan with the patient will include providing facts in the simplest language that the patient and her family will understand. This communication will occur in the presence of the patient and her family and include patient education. I will explain to the patient and her family the need for prevention of type II diabetes in the mother as well as complications related to persistently high.
This communication will explain to the family their role in the patient’s care and demystify common misconceptions about diabetes mellitus treatment in an attempt to improve their decision-making. Assisting the patient and her family in goal setting will encourage participation and this might improve the outcomes of her treatment
Conclusion
The concept map adopts the nursing process to provide a path to the care of the patient. This patient’s needs are educational, emotional, and risk prevention. Her needs require holistic action that would necessitate her family’s involvement in her care and decision-making to enhance the best outcomes. Spiritual, cultural, and patient autonomy are some of the critical factors that would be considered in the communication plan for this patient’s care. Periodical assessment of the quality and safety of the care will be conducted to evaluate the effectiveness of the interventions.
NURS FPX6011 SimmonsC Assessment 1 Evidence-Based Patient-Centered Concept Map References
- Blount, A. (2020). Patient-centered primary care: Getting from good to great (1st ed.). Springer Nature.
- Brown, J. B., Weston, W., & Stewart, M. (2018). Challenges and Solutions in Patient-Centered Care: A case book (J. B. Brown, M. Stewart, & W. W. Weston, Eds.). CRC Press.
- Gomes, D., von Kries, R., Delius, M., Mansmann, U., Nast, M., Stubert, M., Langhammer, L., Haas, N. A., Netz, H., Obermeier, V., Kuhle, S., Holdt, L. M., Teupser, D., Hasbargen, U., Roscher, A. A., & Ensenauer, R. (2018). Late-pregnancy dysglycemia in obese pregnancies after negative testing for gestational diabetes and risk of future childhood overweight: An interim analysis from a longitudinal mother-child cohort study. PLoS Medicine, 15(10), e1002681. https://doi.org/10.1371/journal.pmed.1002681
- Kautzky-Willer, A., Harreiter, J., Winhofer-Stöckl, Y., Bancher-Todesca, D., Berger, A., Repa, A., Lechleitner, M., & Weitgasser, R. (2019). Gestational diabetes mellitus (Update 2019). Wiener klinische Wochenschrift, 131(Suppl 1), 91–102. https://doi.org/10.1007/s00508-018-1419-8
- Liang, H. (2022). The impact of patient-centered care the impact of patient-centered care: Promoting chronic conditions management for older people (1st ed.). Springer.
- Plows, J. F., Stanley, J. L., Baker, P. N., Reynolds, C. M., & Vickers, M. H. (2018). The pathophysiology of gestational diabetes mellitus. International Journal of Molecular Sciences, 19(11), 3342. https://doi.org/10.3390/ijms19113342
- Prabhu J, K., Deepthi Kondamuri, S., Samal, S., & Sen, M. (2021). Knowledge of gestational diabetes mellitus among pregnant women in a semiurban hospital – A cross-sectional study. Clinical Epidemiology and Global Health, 12(100854), 100854. https://doi.org/10.1016/j.cegh.2021.100854
NURS FPX6011 SimmonsC Assessment 1 Evidence-Based Patient-Centered Concept Map Instructions
Create a concept map graphic and write a 2-4 page narrative on the patient scenario presented in Assessment Case Study: Evidence-Based Patient-Centered Concept Map. Base your report on the information provided in the case study and your own research of 3-5 evidence-based resources.
Instructions
Part 1: Concept Map
- Develop a graphical concept map for the patient based on the best available evidence for treating your patient’s health, economic, and cultural needs.
-
- Many organizations use the spider style of concept maps (see the Taylor and Littleton-Kearney article for an example).
- The Assessment Case Study: Evidence-Based Patient-Centered Concept Map, which includes an example of a concept map, may help you prepare your assessment.
- If a particular style of concept map is used in your current care setting, you may use it in this assessment.
Part 2: Narrative Report
- Develop a narrative (2–4 pages) for your concept map.
- Analyze the needs of a patient and his or her family to ensure that the intervention in the concept map will be relevant and appropriate for their beliefs, values, and lifestyle.
-
- Consider how your patient’s economic situation and relevant environmental factors may have contributed to your patient’s current condition or could affect future health.
- Consider how your patient’s culture or family should inform your concept map.
- Determine the value and relevance of the evidence you used as the basis of your concept map.
-
- Explain why your evidence is valuable and relevant to your patient’s case.
- Explain why each piece of evidence is appropriate for the health issue you are addressing and for the unique situation of your patient and the family.
- Propose relevant and measurable criteria for evaluating the outcomes the patient needs to achieve.
-
- Explain why your proposed criteria are appropriate and useful measures of success.
- Explain how you will communicate specific aspects of the concept map to your patient and the family in an ethical, culturally sensitive, and inclusive way. Ensure that your strategies:
-
- Promote honest communications.
- Facilitate sharing only the information you are required and permitted to share.
- Are mindful of your patient’s culture.
- Enable you to make complex medical terms and concepts understandable to your patient and his or her family, regardless of language, abilities, or educational level
Diabetes_Patient_Concept_Map_Scoring_Guide.pdf
Assessment Case Study: Evidence-Based Patient-Centered Concept Map
Concept maps are an important tool in patient–centered care planning. A concept map helps to synthesize facts about a patient’s health needs and personal circumstances with available evidence and analysis. Such a tool becomes more useful when a patient has complex health, economic, and cultural needs.
In this simulation, you will be given a patient to interview and then assemble a concept map for use in that patient’s care plan.
Janie Poole
Charge Nurse
UPTOWN WELLNESS CLINIC
Supervisor Email
You are a nurse at the Uptown Wellness Center. As you begin your shift, you get an email from the charge nurse.
Click the icon to to read it.
Patient Profiles
From: Janie Poole
To: Deshawna Clayton
Good morning,
We have a new patient coming in today.
Her name is Carole Lund. Carole is a new mother who had gestational diabetes during her pregnancy. She has continued to track her blood glucose postpartum, and is worried that it does not appear to be stabilizing.
It probably will be helpful to create a concept map for Carole to show her this care plan in a visual way. Talk to your patient and start planning her care. Thanks!
— Janie Poole
Diabetes Patient
Reason for Referral:
Carole Lund is a 44–year–old woman of mixed Native American and European descent, and a new mother. She is concerned that she is not recovering from gestational diabetes.
Situation:
Carole is here with her daughter, Kassandra, who is 10 weeks old. Carole was diagnosed with gestational diabetes at week 30 of her pregnancy. She has carefully logged her blood glucose since the diagnosis, and it shows 150–200 fasting, over 200 following meals.
Carole Lund
Diabetes Patient Comments:
What diabetes treatments did you receive during your pregnancy?
Well, they gave me a glucometer, so I started using that. I could see right away that the way I was eating was a problem; I would usually work straight through the day and then have one big meal in the evening, and that was making my numbers bounce all over. So I set alarms on my laptop, so three times a day I would get interrupted, have a small meal, take a short walk, and then test my blood sugar. That helped. And then I stopped drinking juice and soda, which I should have done years ago, and that helped too. But I don’t think my numbers improved as much as my OB/GYN wanted them to, but she said my blood sugar should return to normal after delivery.
Did your obstetrician advise you to take insulin during your pregnancy?
She did, yeah, and we talked about it. I don’t like the idea of being dependent on a drug. I called my mother. She’s still on the reservation, so she called the elders, and we all agreed that injecting my body with an animal hormone was a bad idea. But then the doctor told me that they make synthetic insulin now, but that means it’s made in a laboratory somewhere, and I’m not sure that’s any better.
By then I was in my third trimester, and all the tests said Kassandra was big but healthy, so I thought we would just ride it out. It was supposed to clear up after she was born. But it hasn’t, and I know you have to be careful having a baby at my age. I want to do what’s best, but I don’t want to believe that insulin is my only option.
It’s harder now than it was before she was born. It’s just the two of us in the apartment, which is wonderful, but I don’t remember the last time I had a good night’s sleep. A lot of my work is freelance, so I make my own hours, but that also means if I’m not working I don’t get paid. I had family help while I was recovering from the C-section, and they helped cook healthy meals for me, and kept me on my schedule. Now it’s all on me — work, caring for my daughter, and managing my blood sugar. If I fall behind on anything, it will be looking after my health.
Do you have any other concerns you’d like to have addressed?
I worry about Kassandra. She’s healthy and perfect, but I know that she’s at a greater risk for developing Type 2 Diabetes. I want to do whatever I can to reduce that risk, to care for her, and as she grows, to teach her how to care for
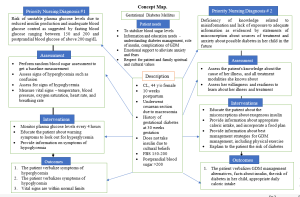
Concept Map
Patient Info:
Name: Carole Lund, 44-year-old female
Native American/European descent
Gestational Diabetes at 30 weeks
Currently at 10 weeks postpartum.
Most Urgent Nursing Diagnosis Name: unstable blood glucose
Most Urgent Nursing Diagnosis Full Description:
- Fasting Blood Sugar 150-200
- Post Prandial over 200
- Cultural belief to not inject animal hormones in body
Most Urgent Nursing Diagnosis Assessment/Diagnostics:
The risk of having an unstable blood glucose level as a result of insufficient blood glucose monitoring is shown by glucose levels that are above the usual range.
Most Urgent Nursing Diagnosis Treatments/Medications:
- Keep an eye on the patient blood glucose levels.
- Inform patients about the signs and symptoms of hypoglycemia and hyperglycemia.
- Create a diet and exercise plan to avoid the need for medication management.
Most Urgent Nursing Diagnosis Outcomes:
- Fasting blood sugars will be less than 130 and after meal blood sugars will be less than 180.
- Confer with a diabetes educator
- Create healthful, simple food plans
4 Participate in some kind of physical exercise.
Nursing Diagnosis 2:
Risk of type 2 diabetes
Nursing Diagnosis 2 Full Description:
A lack of understanding resulting in a misinterpretation of information, as shown by the verbalization of incorrect information.
Nursing Diagnosis 2 Assessment/Diagnostics:
Lack of knowledge about Diabetes
Nursing Diagnosis 2 Treatments/Medications:
- Educate on management of gestational diabetes after delivery
- Educate on diabetes disease process
- Include patient in teaching plan
- Assist patient in incorporating changes into daily routine
Nursing Diagnosis 2 Outcomes:
- Verbalizes understanding of importance of management during postpartum
- Establish diet plan for proper nutrition
- Develop plan for physical activity.
- Patient verbalizes she feels in control of developed action plan
Nursing Diagnosis 3:
Fatigue
Nursing Diagnosis 3 Full Description:
Tiredness caused by sleep deprivation, as shown by a sleep pattern that is not restorative
Nursing Diagnosis 3 Assessment/Diagnostics:
10-week-old baby Single mother “Don’t remember last time I had a good night’s sleep”
Nursing Diagnosis 3 Treatments/Medications:
- Establish bedtime routine
- Educate on the impacts of prolonged sleep deprivation
- Educate on sleeping patterns of babies
- Nap when baby naps
- Seek family to assist with child care support.
Nursing Diagnosis 3 Outcomes:
- Get more sleep by establishing a nighttime schedule and taking a nap every day.
- Explain the relationship between sleep loss and diabetes verbally.
- Establish a timetable for the family to help with child-care responsibilities
Also read: NURS FP6016 SimmonsC Assessment 1 Adverse Event or Near Miss Analysis
